By Angelina Thorne on October 12, 2020
The COVID-19 pandemic has presented medicines optimisation teams with an unforeseen national challenge in delivering new savings programmes. Many CCGs are looking for innovative ways to restart formulary implementation programmes while minimising face-to-face contact with patients.
Currently, medicines optimisation teams often do not have the resources to support primary care teams to audit, review and educate patients about changes that improve patient care and deliver in-year savings. It can be time consuming, and traditionally involved face-to-face interactions at practice and patient level.
Restart – time to change the way we work
Pathways are changing and the way patients access care has shifted providing an opportunity to manage formulary changes more efficiently. Barriers to the use of digital tools and remote ways of working have started to be overcome, paving the way for the use of virtual care models as a valuable addition in managing patient care.
Solutions need to address challenges highlighted by the pandemic
1. Time and resource pressures

Many medicines optimisation staff have been redeployed to support the COVID-19 response and GP practices have limited time to carry out efficiency drives whilst dealing with the back log to maintain patient care in their communities.
Solutions need to ensure minimal impact on time and resources with GP practices still retaining overall control. Support with auditing, selecting and training, both staff and patients, on any changes remotely, will help reduce the burden while continually delivering efficiencies.
2. Patient safety and reassurance

Patient safety remains of paramount importance. So how can this be done where a patient needs product training? In diabetes care, as always, and especially during COVID-19, it’s important to explain what is being changed to ensure medicine adherence and to understand the importance of testing blood glucose levels if people have diabetes.
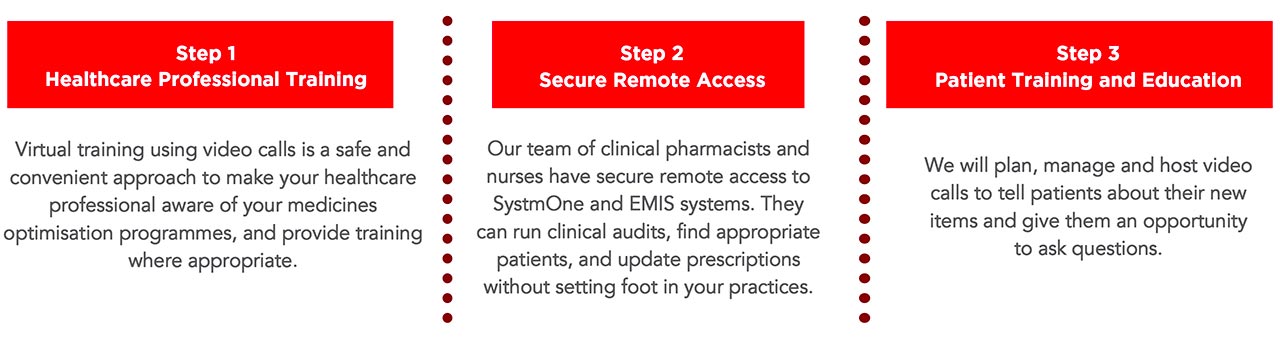
Solutions are now possible using secure remote access to patients. Opportunities to deliver educational training and guidance over the phone, with video calls or face to face if required, can be planned and managed by a specially trained team of clinical pharmacists and nurses. For example, Spirit Implement’s Active Implementation team can run remote clinical audits, find appropriate patients and update prescriptions without needing to set foot in the practices. Working in partnership with the CCG and GP practices, a safe and reliable added value service to support a new product will keep programmes on track and keep both patients and GP staff safe.
3. Data protection, interoperability and governance

Virtual medicines optimisation requires robust systems and data management to ensure security, patient confidentiality and conformance with national and local guidelines, and be compliant with the Data Security and Protection Toolkit.
Solutions must have a robust governance framework, underpinned by a comprehensive suite of policies and procedures, ensuring compliance with the NHS standard contract, local and national guidance, and legislative requirements. Spirit Implement has a proven governance framework and track record in managing implementation programmes. You can read more here.
What does virtual active implementation look like?
Virtual active implementation is a remote medicines optimisation service that respects social distancing.
At Spirit, we use technology to enable “business as usual” from a safe distance, providing you with a 100% remote service, abiding by social distancing rules and eliminating the need for face-to-face contact. It is a model that can be deployed now and going forward as a more efficient way of working.
Getting started
If you would like to review your prescription savings programmes with a trusted partner, please get in touch.
Ref: IMP/3434/OCT20


