By Pash Sonigra on December 15, 2023

The Spirit Health team and I recently attended the Clinical Pharmacy Congress North, held for the first time in the often-rainy city of Manchester.
It’s safe to say that the weather held up to its usual standards for a UK November, but thankfully the conversations held with pharmacists from across the North of the country were much brighter by comparison.

Apart from our very inviting coral-coloured display and the fact we were positioned right next to the main coffee stand (pharmacists sure do love caffeine), one of the reasons we spoke to so many people was due to four tubes and a box full of multicoloured balls.
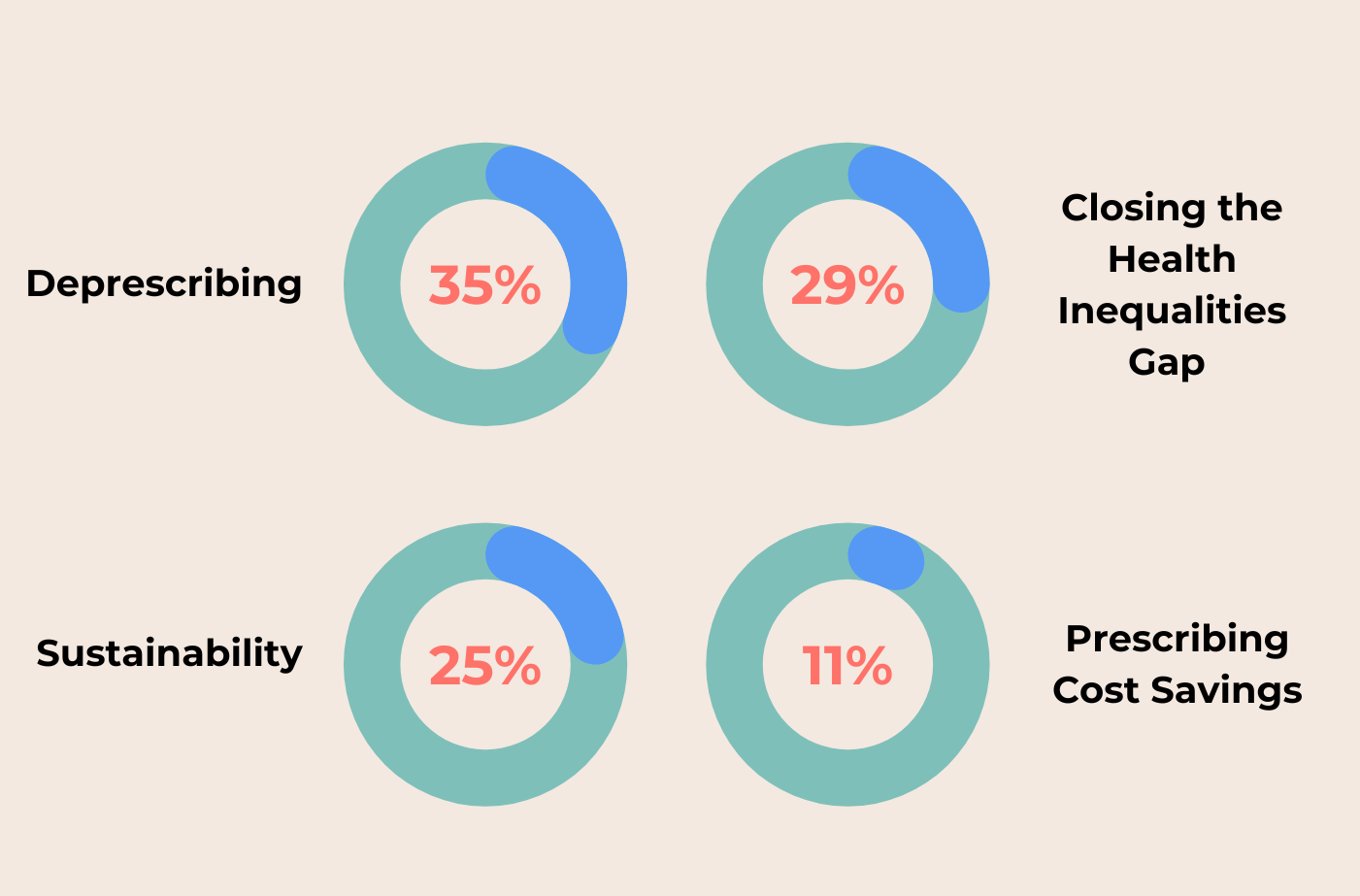
“What do you feel will be the biggest area of focus for Northern medicines optimisation teams in the new 2024/25 financial year?”.
An important question for our guests to vote on. Attendees could only choose one of four clinical priorities;
- Closing the health inequalities gap
- Deprescribing
- Prescribing cost savings
- Sustainable patient care improvement
Given events of this nature are attended by a true mix of NHS professionals (not just the expected primary vs secondary care split), it proved a great chance to gain insight into where people felt the real issues lay within their region.
We carried the poll across both days of the conference, with the results as follows:
Whilst there was often some back-and-forth in conversation between what people felt the NHS should focus on against what they will focus on (somewhat similar to the heart vs head conundrum), the results proved to be interesting. Not necessarily because of where each ball was placed but more so because of the discourse that followed each vote.
Deprescribing
Perhaps unsurprisingly, deprescribing was the much talked-about topic for many of the attendees we spoke to. Regardless of the role each attending pharmacist worked under (PCN, trust, care home, community, locum, trainee, to name a few) all had a story to tell on how polypharmacy was proving to be an issue.
Putting aside the fact that there’s a growing population of patients taking several drugs at any one period of time, it was a blockage of effective communication across different clinical teams that proved the recurring theme. Many told us of their struggle to get authorisation to allow the elimination (or even just reduction) of certain prescribed medicines from a patient’s record, especially when said drugs are being taken for separate clinical conditions. Where an adverse drug reaction is the root cause of a patient’s admission to the hospital/GP, there needs to be a faster, more focused way of communicating between clinical departments to undertake an effective patient review, allowing professionals to pinpoint the cause of the side effects and act accordingly.
Other discussions, usually with primary care pharmacists, fell in line with the nationally stated priorities. Unsurprising, given NHS England’s continued focus on areas such as reducing both national opioid and antidepressant usage (see the latest ‘Medicines Optimisation Opportunities’ list as a key reference). Thankfully, this isn’t a case of ‘how can we save money by reducing the number of drugs being prescribed?’ Specific quality-of-life driven approaches are needed to reduce potential drug addictions/dependencies in the safest & most effective way for patients, regardless of spend input.
Closing the Health Inequalities Gap
Health inequalities, albeit gaining a large percentage of the vote, proved a little more ambiguous in nature.
Given the large-scale transition undertaken when CCGs moved to the ICS structure in July of 2022, reducing the HI gap was seen by voters as remaining vitally important but currently out-of-reach until systems were truly embedded into their new ways of working. A process that will not happen overnight. Many we spoke to mentioned that the funding of local services was still very divided in nature, with the term ‘post-code lottery’ being mentioned on more than one occurrence. Perhaps this coming in second in the poll was a case of heart leading head.
Routes to funding have changed dramatically over the past 18 months, not just where power lies to spend, but the amount of red tape that has to be broken through in order to commission truly equal health opportunities within areas of varying deprivation.
Sustainable Patient Care
Sustainability threw us some interesting opinions.
While the NHS is heavily invested in its green agenda as well as the cause for sustainable improvements to long-term patient care, it was seen as the ‘future’ goal by many. Not something for the here and now that will have an immediate impact on the way the NHS can treat it’s patients.
That leaves us to return to the elephant in the room; money.
Where could these all these new services be funded from? Where could we find the influx needed to promote and fund more sustainable practices that allow access to long-term solutions rather than quick fixes? After all this is a national service that is, if you go by the media, haemorrhaging cash.
Of course, what you hear from the media and what is actually happening are often two very separate things. But that doesn’t mean there’s money to splash on new technology that will overnight equalise health inequalities and perform a national review of medicine usage in the over 65’s.
So, what’s left? Prescribing costs become the focus.
Prescribing Cost Savings
Pharmacy teams are desperate to hit targets, but the fear of it simply become a ‘race to the bottom’ is one that won’t go away.
Yes, we could take the time to switch a cohort of patients from Drug-A to a cheaper Drug-B biosimilar, but when does it stop? Do we do it all again next year when the next pharmaceutical behemoth decides to roll out the new-and-improved version that just so happens to be 10p a pack cheaper than the current market leader? What level of impact is this going to have to the patient if all we chase is cheap?
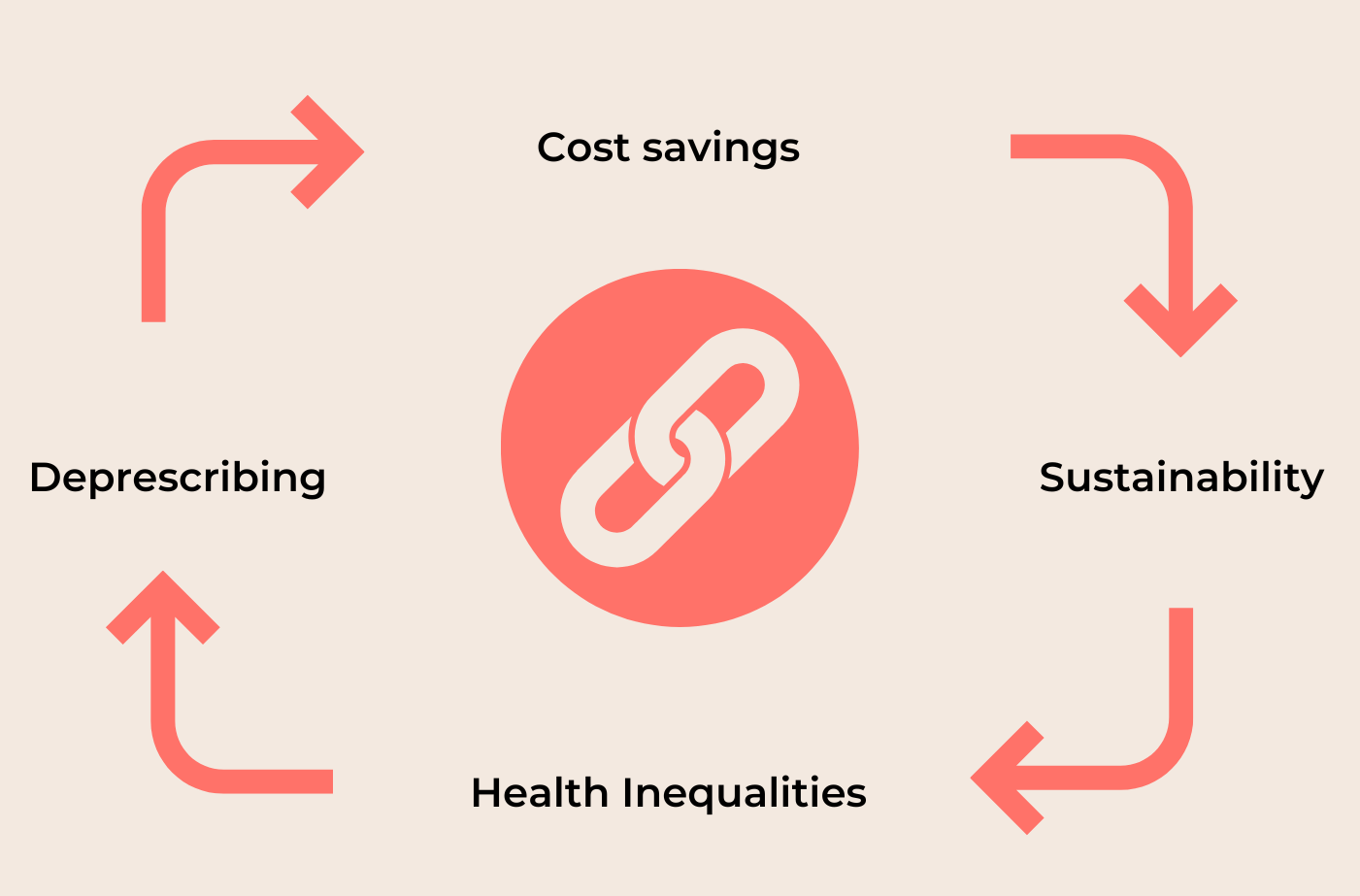
That’s where the links start to form.
Prescribing cost saving is only a short term-win if sustainability isn’t considered.
Can sustainability even exist if people aren’t getting access to the same level of healthcare support regardless of where they live?
It will be much harder for health inequalities be reduced effectively if polypharmacy and high-risk drugs continue their increase in use.
And, of course, deprescribing automatically builds in an efficiency when it comes to cost.
Spirit Health are working hard to provide a range of services that help to cover all four of these essential areas.
What’s next?
If you’d like to hear more about our conversations at CPC North, or you fancy speaking with one of the team about how we can support your region, please contact us here.


