By Steve Marriott on June 11, 2020
Diabetes is a lifelong condition. Due to the ageing population, there will be 20 per cent more cases of Type 2 diabetes in 2036 than there were in 20001. The rising prevalence of diabetes comes with spiralling health care costs. Add the burden from diabetes-related complications, and the costs increase further still. The situation is not sustainable.
Prevention is better than cure, but misinformation enshrines diabetes. Unless we have diabetes or know someone who does, our understanding is likely to be weak. It’s hard to build awareness and encourage healthier lifestyles to reduce the prevalence of diabetes. Temptation surrounds us, and the message often only resonates when it’s too late.
The rise of diabetes seems inevitable. How can the NHS create sustainable cost-efficiencies in the short-term?
The Cost of Diabetes to the NHS
The diabetes.co.uk website cites a series of sobering statistics about the cost of diabetes to the NHS2:
- Diabetes costs the NHS over £1.5 million an hour. That equates to more than £25,000 per minute.
- It estimates the total cost of treating diabetes and its complications is £14 billion a year. Put another way, that’s 10 per cent of the whole NHS budget.
- The NHS spends £172 million on testing supplies such as blood glucose meters, test strips and insulin pen needles.
The Drive to Reduce the Cost of Diabetes to the NHS
Late in 2018, NHS England began a consultation as part of its plan to improve prescribing. The NHS looked at costly items that were working well, but where cheaper options would work well too. The consultation included blood glucose test strips, with these recommendations:
- Not to start new prescriptions for expensive test strips for any new patient.
- To switch existing prescriptions for expensive test strips to lower-cost strips.
The intent was not to stop prescriptions for blood glucose test strips. Instead, the aim was to encourage the use of test strips costing less than £10 per pack of 50. At the time of the consultation, test strips were costing anything up to £17 per pack. Replacing these expensive items with cheaper options that don’t compromise accuracy makes sense. Between October 2017 and October 2019, the national average unit price for test strips has fallen from £12.56 to £11.213.
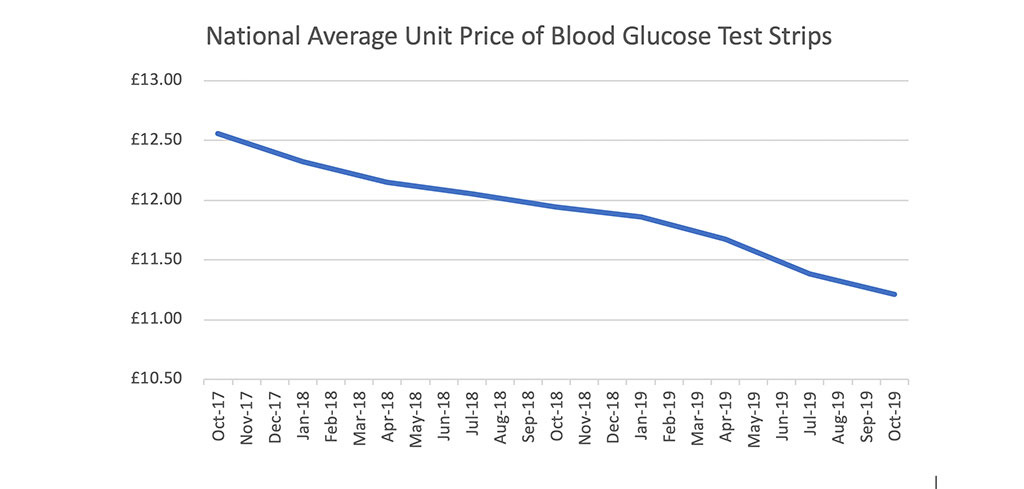
The devil’s in the detail. The general downward trend masks the gap between the best and worst Clinical Commissioning Groups (CCGs). Today, average unit prices for test strips (before locally negotiated rebates) vary from £8.90 to £13.10, and all but 5 CCGs have an average price over £10.00. There’s still a way to go.
Why is it difficult to switch to cost-effective test strips?
Formulary Review Considerations
Even simple switches, such as from one blood glucose test strip to another, take time and effort. CCGs have local formularies of preferred items for every type of medication. There’s an expectation that clinicians will prescribe from the formulary. Sometimes there are legitimate reasons to prescribe off-formulary medications though, such as when:
- a patient had received the formulary item before but stopped using it due to poor response or intolerance
- the patient has an allergy to an ingredient
- there is uncertainty about the patient’s suitability for the switch. For example, they might live alone and have a visual impairment
During a formulary review, a CCG medicines optimisation team compares available products. It’s normal for them to choose several options to include on the formulary. This decision isn’t about price alone. Considerations will often also include continuity of supply, clinical effectiveness and quality. As John Ruskin said:
“There is hardly anything in the world that some man cannot make a little worse and sell a little cheaper, and the people who consider price only are this man’s lawful prey.”
Deciding which products should be on the formulary is only the start of the process. Merely changing the items on the formulary won’t save a single pound. Hard work at GP practices unlocks the cost reductions. Every practice will need to:
- audit the computer records to identify suitable patients that have prescriptions to switch
- conduct a clinical review of each of these patients
- authorise the switches
- update the prescription item on each patient’s medical record
- send letters to each patient to tell them about the medication change
Formulary switches can be a painful process for practice staff. Primary care is under pressure, and formulary switches create more work at practices. Changing medication can cause angst for patients too. Many people don’t like change, especially when it might impact their health.
Introducing Active Implementation
What if someone could do the work for practice staff? Wouldn’t it be great if someone could spend time with patients to discuss the change to their test strips? That’s what we do at Spirit Health. We call it active implementation. We work with CCGs, GP practices and patients to make change happen. There are many benefits of active implementation:
- easing the pressure and relieving the workload at practices;
- improving the quality of care and patient outcomes; and
- quicker realisation of cost savings.
We follow best practice in medicines optimisation. Clinical pharmacists and nurse educators work together to focus on the needs of the CCG, its clinicians and patients. They build a three-tiered change programme of support and education:
Tier 1: Product Training for Healthcare Professionals
Patients will turn to practice nurses and local pharmacists when they need help with their new meters and strips. This training allows nurses and pharmacists to answer questions straight away with confidence.
Tier 2: Practice Audits
Audits of the medical records at each GP practice finds suitable patients for review. A nominated GP authorises the recommended interventions.
Tier 3: Patient education
Showing patients how to use their new meters and test strips is an essential aspect of the programme. Small group sessions (or one-to-one meetings if required) work well. Patients are more at ease. They like small group discussions and the opportunity to ask questions. These clinics are an opportunity to discuss diet, lifestyle and exercise too.
The Proven Impact of Active Implementation
Practical training, support and education during formulary changes have a significant impact on the cost reductions. NHS Bury CCG and NHS Heywood, Middleton and Rochdale CCG recently switched to more cost-effective blood glucose test strips. The changeover included an active implementation programme. The resulting drop in the cost of test strips gathered momentum in line with the increasing use of the new cost-effective strips:
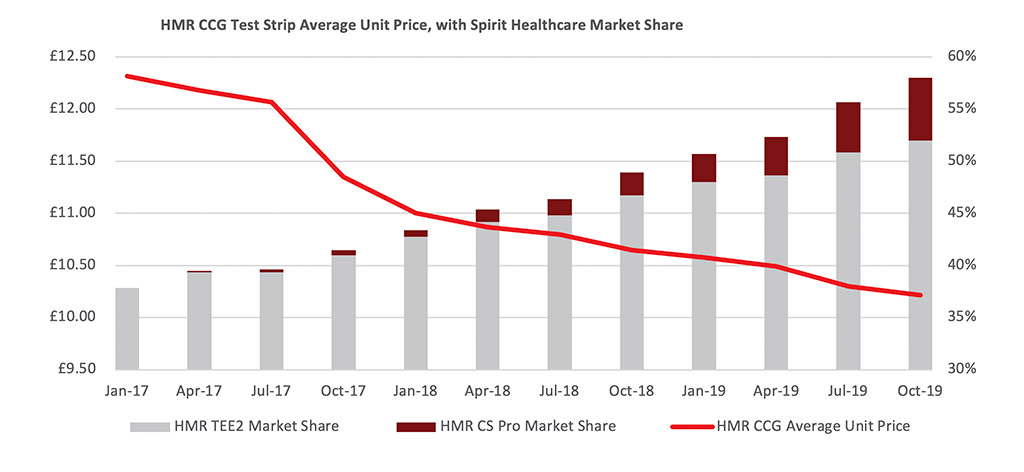
A study in formulary changes for diabetes showed that savings were almost 700 per cent greater with an active implementation, compared to similar CCGs with no implementation programme.
In December 2017, NHS Isle of Wight CCG reviewed its blood glucose meters and test strips. Training courses held at GP practices across the island were an integral part of the change programme. In the first six months, the CCG’s average unit price of test strips fell by £2.34.
The cost savings from switching to cost-effective test strips with active implementation can be significant. Annualised savings in NHS Heywood, Middleton and Rochdale CCG equated to £154,1204.
Time to Change
The standard and cost of blood glucose test strips vary across the NHS. An active implementation approach to formulary change can take a CCG from having one of the highest unit costs of test strips to being amongst those with the lowest.
CCGs are under increasing pressure to spend less on test strips without compromising quality. It’s time to recognise best practice and adopt active implementation for formulary changes. It’s an effective way to reduce the cost of diabetes to the NHS.
References
1 Bagust, A., Hopkinson, P.K., Maslove, L. and Currie, C.J. (2002), The projected health care burden of Type 2 diabetes in the UK from 2000 to 2060. Diabetic Medicine, 19: 1-5. doi:10.1046/j.1464-5491.19.s4.2.x
2 https://www.diabetes.co.uk/cost-of-diabetes.html
3 Data on file
4 Swift, J., Pearson, K., Hill, J., Cheung, J., Richardson, D., Myers, A.J. and Barker, C. (2017) Implementing formulary change in diabetes. British Journal of Healthcare Management, Vol 23, No. 4 https://doi.org/10.12968/bjhc.2017.23.4.167