By Sophie Davis-Cooper on October 19, 2021
A new comprehensive guide from the Quality Compliance Systems (QCS) and the National Care Forum (NCF) has been created to help the care sector get ‘winter ready’, as the UK enters a second wave of the coronavirus pandemic, as well as a potential increase in influenza cases this winter.
In order to get prepared and protect service users from hospitalisation, the report, which is broken down into four sections, offers care staff easy-to-read fact sheets, templates and infographics to understand how to manage the dual burden of winter flu and COVID-19.
During the peak of the pandemic, the 2020 NHS Framework for Enhanced Health in Care Homes recognised remote monitoring as an opportunity to enhance the quality of care for residents. More recently, the Department of Health and Social Care has warned care homes in England of a rise in infections, urging bosses to take the necessary actions to prevent and limit outbreaks.
Digital, remote monitoring healthcare technology is a proven method that allows care home residents to be regularly assessed to ensure this continuity of care while keeping vulnerable and shielding patients safe. In this article, we explore how Spirit Health can help to support each of the areas highlighted by the QCS and NCF, allowing both staff and residents in care homes to benefit from remote monitoring technology.
Information and Technology
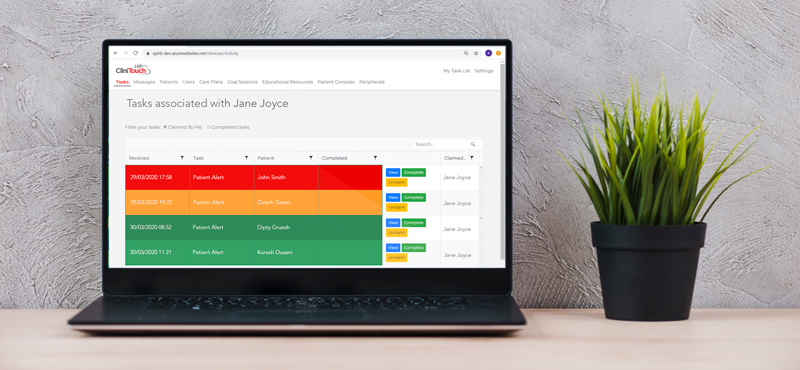
Remote monitoring technology, such as Spirit Health’s CliniTouch Vie, allows real-time biometric and wellbeing data to be collected and entered into the digital platform for residents by the patients’ carers in the home.
Assessments are done by carers who will take patients’ vital signs readings and answer personalised and simple health questions. These readings are clinically validated and supported by sophisticated algorithms to give a risk assessment to the GP who is responsible for the day to day care of these vulnerable individuals.
This technology enables GPs to be presented with important clinical information on their patients quicker and faster than they would do in a traditional setting, which can then be monitored and form an integral part of the patient’s care plan.
Infection Prevention and Control
Extending the concept of the care home to one akin to a ‘virtual ward’, the real-time information now available to both GPs and care home staff allows them to rapidly assess a patient and respond at the outset of any symptoms or deterioration. Clinical teams can become more efficient in how they address infections, access medications and ensure the continuity of care for patients with long-term conditions.
Moreover, having immediate access to a dashboard of live clinical data on a group of patients enables rapid identification and triage of those individuals most at risk, allowing teams to both prevent and control any problems before they arise.
GPs can also amend the care plans of individual patients with specific medical requirements to be monitored more frequently, while carers can also instigate an immediate virtual ward round to address specific concerns as they arise. By having this frequent and consistent medical insight, care can be maintained throughout the care home.
Planning and Supporting Safe Hospital Discharge

Not only does this proactive model of care allow for early intervention that helps keep people out of the hospital, but it also enables earlier, safe hospital discharge by connecting multi-disciplinary care teams, including responsible community-based healthcare professionals. Moreover, it increases health system capacity and reduces the risk of cross-contamination at a time when our collective focus is on protecting our vulnerable and our NHS.
CliniTouch Vie can help to empower carers and patient self-management through a managed, holistic care model that supports patients within their care home or home setting. By being able to remotely connect with a GP and/or community practitioner, patients have access to health and wellbeing advice, as well as having comfort in knowing that a healthcare professional can intervene where and when more urgent care is needed.
Workforce Wellbeing

During the onset of COVID-19, GP practices across the UK were facing increased demand for delivering primary care for their patients in care homes. Both care homes and GP practices struggled to find solutions that provided care that was safe for patients, carers and clinicians.
Remote monitoring solutions help care home teams manage their time and resources more effectively. Workforces can make better use of their time, as remote monitoring technology presents a tangible opportunity for care home staff to care holistically and consistently for their residents.
Beforehand, carers were often faced with the difficult decision of whether a resident’s condition required more urgent intervention, such as calling out a GP or making the choice as to whether the issue could wait to be addressed. Especially during the pandemic, those decisions become even more difficult because of the heightened duty of care to keep residents safe and minimise the pressure on local health services. Remote monitoring technology removes this guesswork by being able to improve the speed of communication between carers and GPs, as well as having insight into patients who are high-risk in order to prioritise and make more informed decisions.
The result is improved relationships between all stakeholders on the care continuum, reduced stress levels, and, ultimately, better, safer working environments.


